Beyond the Exam Room
Five alumni, who also have medical degrees and are working across different corners of healthcare, share candid insights on where the nation’s healthcare system is headed, the promises of new technologies and the pitfalls that must be addressed for lasting reform.
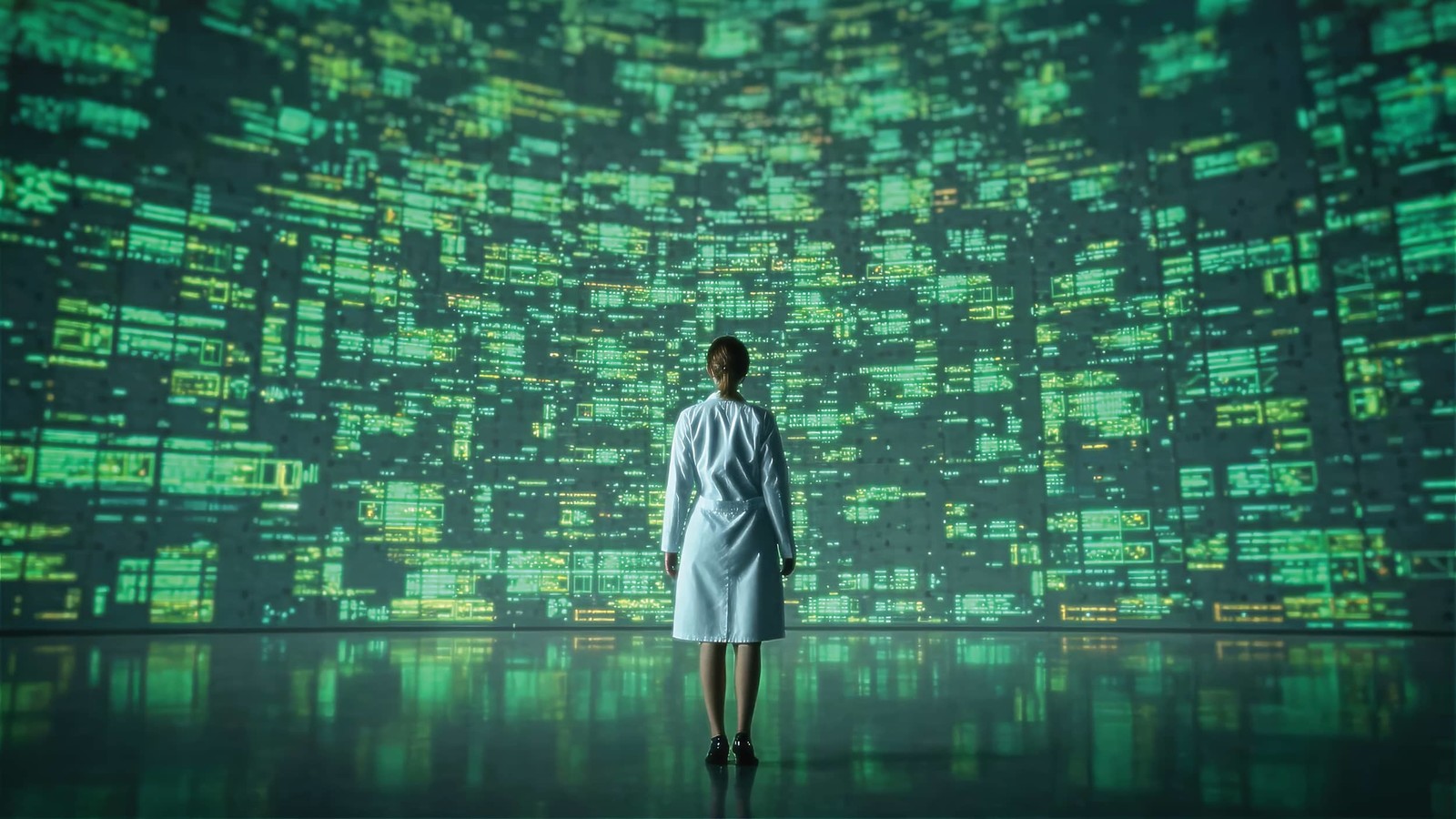
There is a broad trend in healthcare leadership — the growing recognition that clinical excellence alone isn’t enough to navigate modern medicine’s complex challenges. Artificial intelligence, physician burnout and financial sustainability aren‘t abstract policy debates for the doctors on the front lines. They’re daily realities shaping how care is delivered — and how patients experience medicine.
Rice Business has emerged as a natural hub for this evolution, positioned in the heart of the world’s largest medical center. The school’s dual-degree program, pairing the Rice MBA with a medical degree from Baylor College of Medicine, prepares future physician-leaders to tackle healthcare’s multifaceted problems from day one. Meanwhile, the proximity to the Texas Medical Center draws established physicians to Rice’s Executive MBA program, where they gain the business acumen to drive systemic change in their organizations. “Our alumni with MDs are uniquely positioned to help shape the future of healthcare,” says Shiva Sivaramakrishnan, academic director of healthcare programming and the Henry Gardiner Symonds professor in accounting at Rice Business. “They combine firsthand clinical experience with the big-picture strategic thinking needed to tackle systemic challenges facing healthcare — from financial sustainability to technological innovation and workforce well-being.”
Whether earned alongside medical training or years into practice, the MBA becomes a powerful lens for seeing healthcare not just as a calling, but as a complex system that can be redesigned, optimized and ultimately healed.
The AI Revolution: From Burden to Benefit

When electronic medical records (EMRs) first rolled out, many physicians saw them as one more bureaucratic hurdle. “Despite physicians complaining about electronic medical records adding time and cognitive burdens, no doctor would choose to work without them,” says Dr. Anita Ying, EMBA ’13, vice president of ambulatory and revenue cycle medical operations at MD Anderson Cancer Center.
Now, artificial intelligence is beginning to smooth out the rough edges. At MD Anderson, ambient listening technology automatically generates clinical notes from patient visits. “I can focus entirely on my patients,” Ying explains. “I still review and edit the draft, but the cognitive load is dramatically reduced.” Those notes simultaneously serve colleagues coordinating care, meet billing requirements and update patients through their online portal.
Ying sees even broader potential: AI-powered tools could analyze events during a patient’s hospital stay to identify potential safety gaps for clinicians, while large language models could streamline back-office tasks like billing. Telemedicine, too, has reshaped care since COVID. Before the pandemic, virtual visits were rare. Today, 20% of MD Anderson’s outpatient appointments are remote, saving patients travel costs and time away from work. Still, Ying warns that without interstate licensure reform and more comprehensive reimbursement models, the promise of telemedicine will remain incomplete.
Burnout at a Breaking Point

If AI offers hope, the human toll of modern healthcare remains sobering. Dr. Aparajitha K. Verma, EMBA ’18, medical director of quality and patient experience at UTHealth Houston Neurosciences, describes physician burnout as “a persistent, progressive crisis.” Causes range from endless administrative tasks to rigid schedules that leave no space for work-life balance.
Some solutions are technological — AI scribes that take notes, tools that triage inboxes. But Verma insists that technology alone isn’t enough. “There needs to be fundamental cultural and policy changes led by healthcare organizations,” she says. She argues for aligning incentives with physician values, shifting compensation from volume to value, investing in leadership pathways and offering mental health support without stigma. “The goal is to reconnect physicians with their original purpose,” she adds, “while providing the flexibility and support they need to thrive.”

Dr. R. Jason Yong, MD/MBA ’08, chief of the Division of Pain Medicine at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, echoes those concerns. He sees burnout as a form of “moral injury” — a widening gap between why physicians entered medicine and what their days actually look like.
Here too, AI offers a counterweight. Machine learning can uncover treatment insights from vast datasets. More transparent approaches, such as relevance-based prediction models, show physicians how conclusions are reached — preserving both accuracy and trust. Chatbots and AI-driven intake systems can also streamline visits, allowing doctors to spend more meaningful time with patients. “If designed thoughtfully,” Yong stresses, “AI can help restore what drew many of us to medicine in the first place: caring for patients face-to-face.”
Access and Equity: The Upstream Challenge

While technology and burnout capture headlines, Dr. Omar Matuk-Villazon, EMBA ’18, chief medical officer at Suvida Healthcare, sees a more fundamental crisis brewing. Physician shortages aren't just numbers on a spreadsheet — they’re reshaping who gets care and how. At Suvida, a value-based primary care organization serving Latino seniors, those shortages translate directly into health disparities.
“For these patients, a shortage doesn’t just mean waiting longer for an appointment,” Matuk- Villazon explains. “It can mean worsening chronic disease and unnecessary ER visits.” Language barriers, cultural mistrust and geographic isolation compound the problem. Rural hospital closures leave entire communities stranded, while emergency department overcrowding becomes “simply the downstream signal of upstream failure.”
His Rice MBA training taught him to see these challenges structurally, not just clinically. “We cannot solve shortages with numbers alone,” he says. “We must redesign delivery — building team-based models where physicians, nurse practitioners and community health workers extend one another’s reach, supported by technology.” The vision goes beyond traditional brick-and-mortar thinking.
“Access is no longer just about hospitals; it’s about continuity, cultural trust and the right care at the right time.”
For Matuk-Villazon, the business challenge is clear: aligning incentives so that equity becomes financially sustainable. “When we succeed, we create not just access, but equity — and that is the foundation for healthier communities.”
Dollars and Diagnosis: The Economic Tension

Beyond technology and workforce well-being, the economics of healthcare threaten its foundation. “The biggest challenge in healthcare today is financial sustainability,” says Dr. Rupesh Nigam, EMBA ’23. Costs continue to rise faster than wages, leaving families vulnerable to debt and health systems under pressure. Even insured patients face medical bankruptcy.
Nigam points to a deeper problem: healthcare is trapped between fee-for-service, which rewards volume, and value-based care, which rewards outcomes. The result is an unstable middle ground. “This tension makes it harder to plan, invest and deliver care efficiently,” he explains. The ripple effects are visible at the bedside: delayed discharges, fragmented coordination and avoidable readmissions — all costly, all corrosive to trust.
For Nigam, sustainability depends on treating healthcare both as a service and as a business. “We need to simplify processes without sacrificing quality, use technology to reduce waste, and build stronger alignment among payers, providers and patients,” he says. Only then can financial reality and clinical mission converge.
Where Medicine Meets Management
Across these perspectives, one theme stands out: Technology alone won’t heal healthcare, but it can be a catalyst for change. AI can lighten documentation burdens, extend the reach of specialists through telemedicine and make visits more human. But unless health systems also reform outdated structures, invest in their people and reconcile competing payment models, progress will remain piecemeal.
For physicians like Ying, Verma, Yong, Matuk-Villazon and Nigam, the vision is clear. Healthcare must evolve into a system where innovation, sustainability and humanity reinforce — rather than undermine — one another. That, they argue, is the prescription for a healthier future.